Rat Lungworm Overview

 The nematode Angiostrongylus cantonensis is a rat lungworm, a zoonotic pathogen which causes a global, emerging infectious disease known as angiostrongyliasis or rat lungworm disease (RLWD). This nematode was first discovered in China in 1935 1, but is now endemic in Asia, Australia, the Caribbean islands and Pacific islands. It has also spread to the American continents and can be found in the continental U.S. along the Gulf Coast from Florida into Texas and up into Tennessee and Oklahoma 2. More than 2,800 cases of human infection were reported in 30 countries in a 2008 paper, however the number has grown. 3 4. In Hawaiʻi alone, from 2007 to 2017, 82 cases of angiostrongyliasis have been reported and it is agreed upon by the Hawaiʻi Department of Health that cases are under-reported 5.
The nematode Angiostrongylus cantonensis is a rat lungworm, a zoonotic pathogen which causes a global, emerging infectious disease known as angiostrongyliasis or rat lungworm disease (RLWD). This nematode was first discovered in China in 1935 1, but is now endemic in Asia, Australia, the Caribbean islands and Pacific islands. It has also spread to the American continents and can be found in the continental U.S. along the Gulf Coast from Florida into Texas and up into Tennessee and Oklahoma 2. More than 2,800 cases of human infection were reported in 30 countries in a 2008 paper, however the number has grown. 3 4. In Hawaiʻi alone, from 2007 to 2017, 82 cases of angiostrongyliasis have been reported and it is agreed upon by the Hawaiʻi Department of Health that cases are under-reported 5.
Rats are the definitive host, primarily Rattus spp. All three species of rats found in Hawaiʻi (R. rattus, R. norvegicus, and R. exulans) are capable of acting as definitive hosts 6 7. When rats eat infected slugs or snails, they ingest third stage (L3) larvae which eventually grow to sexual maturity. The male and female worms reproduce in the heart, pulmonary artery, and lungs of the rat 8. Fertilized eggs hatch in the lungs of the rat, thus the term rat lungworm disease. The newly hatched first stage larvae (L1) migrate up the bronchial tree, are swallowed, and are excreted with feces. The timeline, from when the rat eats a slug/snail with the L3 larvae, to excreting L1 larvae in feces, is 6 – 8 weeks 9.
Slugs and snails are the obligatory intermediate host and support parasite development from the L1 to the L3 larval stage. By eating infected rat feces, the slug or snail acquires the L1 larvae. Once ingested, the L1s settle into tissue and in about 12 days will molt without shedding, becoming a second stage (L2) larvae. The L2s go through the second molt, again without shedding, becoming L3 larvae on the 17th to 21st day. While the length of time it takes for the larvae to develop from an L1 into an L3 is about three weeks, the L3 larvae have been shown to survive in a snail host for up to 12 months with no apparent effect on the snail 10. They simply wait for the rat to eat the slug to complete the rat lungworm lifecycle.
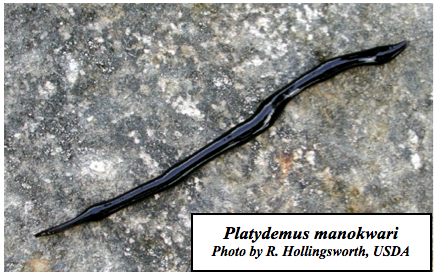 Humans and other animals, such as dogs, horses, apes, monkeys, and some bird species, are accidental hosts. They become infected by ingesting intermediate (slugs/snails) or paratenic (passive carrier) hosts containing infective L3 larvae. The most important paratenic hosts are crustaceans, such as shrimp, prawns and land crabs, and predacious land planarians, such as flatworms in the genus Platydemus 11. Centipedes, frogs, and some types of lizards are also paratenic hosts 3 11 12.
Humans and other animals, such as dogs, horses, apes, monkeys, and some bird species, are accidental hosts. They become infected by ingesting intermediate (slugs/snails) or paratenic (passive carrier) hosts containing infective L3 larvae. The most important paratenic hosts are crustaceans, such as shrimp, prawns and land crabs, and predacious land planarians, such as flatworms in the genus Platydemus 11. Centipedes, frogs, and some types of lizards are also paratenic hosts 3 11 12.
Once ingested by humans, larvae penetrate the intestinal mucosa and travel through the liver and lungs to the central nervous system (CNS) 3. RLWD can be a serious threat to human health. Angiostrongyliasis in humans can result in transient meningitis (inflammation of the meninges of the brain and the spinal cord) or a more serious disease involving the brain, spinal cord and nerve roots, with a characteristic eosinophilia of the peripheral blood and cerebrospinal fluid 13. Humans are a “dead-end” host, meaning the parasites do not reproduce in humans but remain in the CNS or can move to the eye chamber causing ocular angiostrongyliasis, where they remain until parasite death 4.
 A. cantonensis has been documented as a parasitic disease of humans in Hawaiʻi and other Pacific islands since the early 1960’s 14. The flatworm Platydemus manokwari and the semi-slug Parmarion martensi (hereafter referred to as semi-slug) had recently immigrated to Japan and were thought to be the probable cause of an outbreak of angiostrongyliasis there in the year 2000 15. The semi-slug is also a recent immigrant to the Hawaiian Islands 16 and is thought to be responsible for a recent outbreak of angiostrongyliasis cases on the Island of Hawaiʻi 17.
A. cantonensis has been documented as a parasitic disease of humans in Hawaiʻi and other Pacific islands since the early 1960’s 14. The flatworm Platydemus manokwari and the semi-slug Parmarion martensi (hereafter referred to as semi-slug) had recently immigrated to Japan and were thought to be the probable cause of an outbreak of angiostrongyliasis there in the year 2000 15. The semi-slug is also a recent immigrant to the Hawaiian Islands 16 and is thought to be responsible for a recent outbreak of angiostrongyliasis cases on the Island of Hawaiʻi 17.
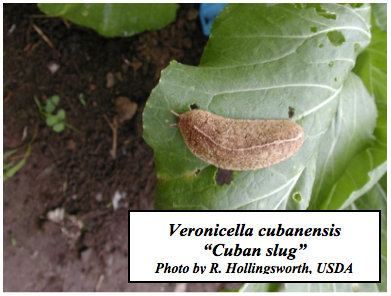 In the district where the disease outbreak occurred (Puna district of the Island of Hawaiʻi), >75% of P. martensi were found to be infected with A. cantonensis. In certain areas, semi-slugs were very numerous and some were heavily infected with L3 A. cantonensis larvae 17.
In the district where the disease outbreak occurred (Puna district of the Island of Hawaiʻi), >75% of P. martensi were found to be infected with A. cantonensis. In certain areas, semi-slugs were very numerous and some were heavily infected with L3 A. cantonensis larvae 17.
-
Chen HT. Un nouveau nematode pulmonaire, pulmonema cantonensis, NGN sp. Des rats de Canton. Ann Parasit Hum Comp 1935;13:312.
-
Flerlage T, Qvarnstrom Y, Noh J, Devincenzo JP, Madni A, Bagga B, Hysmith ND, 2017. Angiostrongylus cantonensis eosinophilic meningitis in an infant, Tennessee, USA. Emer Infect Dis. 23(10): 1756-1758. DOI: 10.3201/eid2310.170978
-
Wang QP, Lai DH, Zhu XU, Chen X-G, Lun ZR. Human angiostrongyliasis. Lancet Infect Dis 2008;8:621-630.
-
Wang QP, Wu ZD, Wei RL, Owen ZR, Lun ZR. Human Angiostrongylus cantonensis: an update. Eur J Clin Microbiol Infect Dis 2011;DOI 10.1007/s10096-0111328-5.
-
Johnston, DI. Dixon, MC, Elm Jr, JL,, Calimlim, PS, Sciulli, RH, Park, SY. 2019. Review of cases of angiostrongyliasis in Hawaii, 2007-2017. Am. J. Trop. Med. Hyg. doi:10.4269/ajtmh.19-0280
-
Martin-Alonso A, Foronda P, Quispe-Ricalde MA, Feliu C, Valladares B. Seroprevalence of Angiostrongylus cantonensis in Wild Rodents from the Canary Islands. PLoS ONE 2011;6(11): e27747. doi:10.1371/journal.pone.0027747
-
Jarvi et al 2017 Plos One’ or ‘Niebuhr et al. 2021 Parasitology’ work
-
Alicata JE, Jindrak K. Angiostrongylosis in the Pacific and Southeast Asia. Charles C. Thomas, Springfield, Illinois. 1970.
-
Wu GH. Angiostrongylus cantonensis. In: Tang JQ ed Nature-borne diseases Science Press Beijing p 1182. 2006.
-
Richards and Merrit. 1967. Studies on Angiostrongylus cantonensis in molluscan intermediate hosts. The Journal of Parasitology. 53(2): 382-388.
-
Hollingsworth RG, Kaneta RK, Sullivan JJ, Bishop HS, Qvarnstrom Y, da Silva AJ, Robinson DG. Distribution of Parmarion cf. martensi (Pulmonata: Helicarionidae), a new semi-slug pest on Hawaii Island, and its potential as a vector for human angiostrongyliasis. Pacific Sci 2007;61:457-468.
-
Barratt et al. 2016. Angiostrongylus cantonensis: a review of its distribution, molecular biology and clinical significance as a human pathogen. Parasitology. 143: 1087-1118. DOI: 10.1017/S0031182016000652
-
Neibuhr CN, Jarvi SI, Kaluna L, Torres Fischer BL, Deane AR, Leinbach IL, Siers SR. 2020 Occurrence of rat lungworm (Angiostrongylus cantonensis)in invasive coqui frogs (Eleutherodactylus coqui) and other hosts in Hawaii. Journal of Wildlife Diseases. DOI: 10.7589/2018-12-294
-
Kliks MM, Palumbo NE. 1992. Eosinophilic meningitis beyond the Pacific basin: the global dispersal of a peridomestic zoonosis caused by Angiostrongylus cantonensis, the nematode lungworm of rats. Soc Sci and Med. 34:199-212.
-
Wallace GD, Rosen L. 1969. Studies on eosinophilic meningitis V. Molluscan hosts of Angiostrongylus cantonensis on Pacific Islands. Am J Trop Med Hyg. 18:206-216.
-
Asato R, Taira K, Nakumura M, Kudaka J, Itokazu K, Kawanaka M. 2004. Changing epidemiology of Angiostrongyliasis cantonensis in Okinawa Prefecture, Japan. Jpn J Infect Dis. 57: 184-186.
-
Cowie RH. 1997. Catalog and bibliography of the nonindigenous nonmarine snails and slugs of the Hawaiian Islands. Bishop Museum Occasional Papers. 50:1-66.

